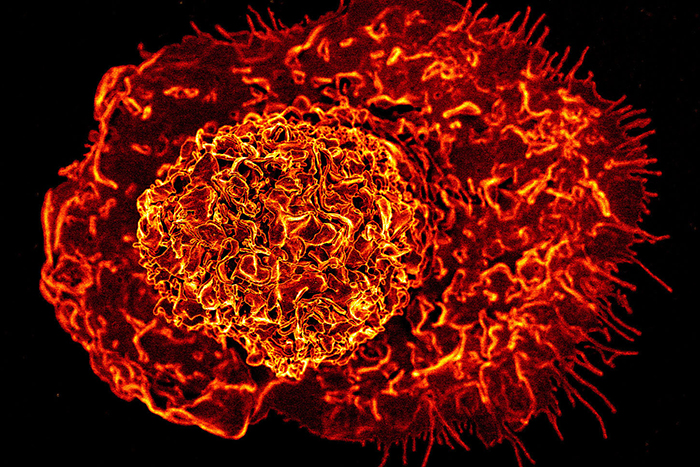
Macrophages like this one help protect the body from pathogens and other external. Photo courtesy of NIH/NIAID
Our immune system contains many types of cells that help protect the body against disease. One type, called macrophages, are cell-eating machines that engulf and digest bacteria, viruses and other threats. The activity of macrophages can impact the outcome of virtually any disease, but scientists are still working to learn how they behave in different diseases and how we can use this knowledge to develop new treatments.
Researchers at University of California San Diego School of Medicine are now using machine learning to help answer this question. They identified a group of genes, which they call SMaRT genes, that can be used to predict the outcome of various diseases based on how these genes are expressed in macrophages. The study was published July 27, 2023 in eBioMedicine.
Macrophages are found throughout the body, but they look and act very differently in different organs and disease contexts. These differences have made it difficult to discover new treatments that target macrophages
“While the era of single cell biology has focused on the myriad of ways tissue macrophages differ from each other, this work shows that underneath such differences, macrophages anywhere and everywhere are fundamentally quite similar,” said first author Pradipta Ghosh, MD, professor and director of the Institute for Network Medicine at UC San Diego School of Medicine.
In response to threats, macrophages have two main responses: they can either promote inflammation, or decrease inflammation and promote tissue repair. Using machine learning, the researchers identified a group of 338 genes that together control which of these two responses occur and how extreme that response is.
They then used these genes to develop a scoring system that measures the inflammatory activity of macrophages. Using existing patient data from a variety of diseases, including sepsis, liver fibrosis and several cancers, they found that the score was an accurate predictor of disease outcomes. For example, tumors with higher scores, indicating more inflammation, consistently carried a worse prognosis than those with lower scores, even in completely different types of cancer.
They also found that diminishing or enhancing the activity of specific SMaRT genes resulted in predictable changes in macrophage activity, suggesting that these genes could help guide the discovery of new therapies that target the immune system.
The researchers are optimistic that their study could prove a major landmark in the field of macrophage biology. In support of these findings, the team has received a $5 million award from the National Institute of Allergy and Infectious Diseases to continue this line of research.
— Miles Martin