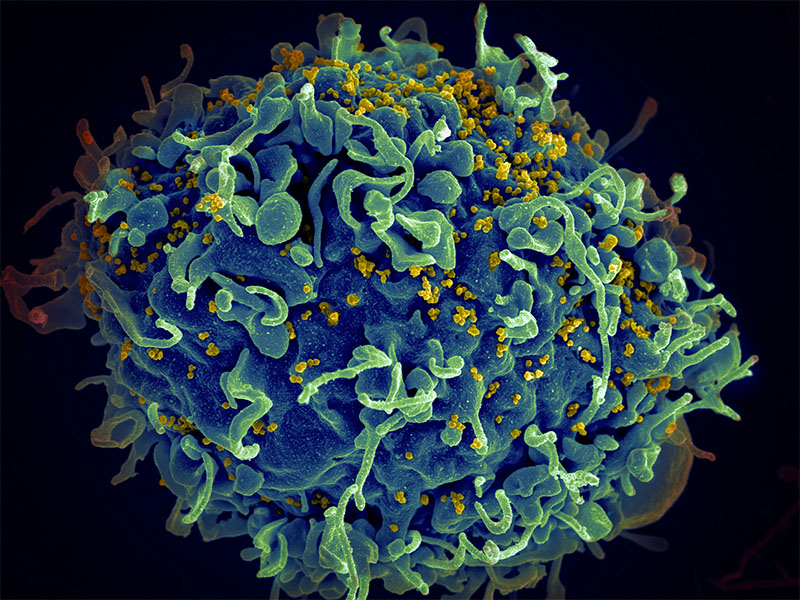
The HIV virus, shown here in yellow, infects cells of the immune system, making people more vulnerable to common infections like cytomegalovirus (CMV). Treating coinfections like CMV could help reduce chronic complications linked to HIV. Photo credit: NCI
Researchers from the HIV Institute at the University of California San Diego School of Medicine recently presented new data about a promising treatment targeting cytomegalovirus (CMV), a virus found in most people living with HIV. While people being treated for HIV rarely experience direct symptoms of CMV, the virus is thought to trigger background immune responses that increase the risk of heart disease and other chronic conditions.
The new research, presented at the Conference on Retroviruses and Opportunistic Infections on March 6, 2023, confirms this hypothesis and suggests that by treating CMV, it may be possible to reduce inflammatory pathways which have been causally linked to aging-related complications in people with HIV. The researchers completed the work as part of the AIDS Clinical Trial Group, a global network of scientists that conducts research to improve the management of HIV and its comorbidities.
CMV is present in about 60% of the general population and 95% of people living with HIV. Before antiretroviral therapies (ART) became available for HIV in the late 90’s, CMV caused life-threatening infections in the eyes, brain, and gut in people with advanced AIDS. While the immune system recovery resulting from ART has rendered this type of CMV organ disease rare, CMV has evolved many mechanisms to modulate immune responses even when it is not causing obvious symptoms.
In the new study, the researchers gave participants with HIV undergoing ART another drug called letermovir, which the team hypothesized could suppress HIV-related inflammation that contributes to chronic diseases. The researchers found that letermovir reduced many important inflammatory pathways and reduced the amount of CMV shed by participants in both oral and genital fluids.
The research team is considering a follow up study to advance this therapeutic pathway.
“I have dedicated most of my career so far investigating the interplay between CMV, HIV and the immune system. Until now, however, we were never able to prove that CMV is causally associated with inflammation and aging-related complications. This clinical trial was successful at clarifying some of the underlying mechanisms,” said study co-lead Sara Gianella Weibel, M.D., associate professor of medicine at UC San Diego. “It’s too soon to say whether or not this approach will tangibly reduce the risk of chronic conditions associated with CMV and HIV, but we’re excited by the possibilities this new data presents.”
— Miles Martin